Transitional Reinsurance Program Fee Filing Service
Employers who sponsor minimum value, self-funded health plans are required to report membership data to the Centers for Medicare and Medicaid Services (CMS), and schedule payments for the Traditional Reinsurance Program (TRP). Membership data needs to be reported by Nov. 16th, 2015.
Benefit Comply offers a reporting service for employers who need help with this process. Benefit Comply will collect the information necessary and complete the entire reporting process for the employer other than entering company banking information needed to make payments. Benefit Comply will then assist the employer in entering their own banking information and scheduling payment. With Benefit Comply’s assistance the entire process will only take the employer a few minutes to complete.
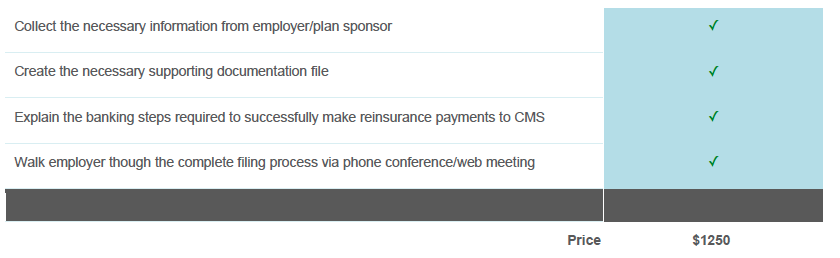
Further discounts available for retainer clients and members of partner organizations.
To start the process, submit the information we will need to assist you.
Note: The Benefit Comply Filing Service assumes the employer already knows what membership total needs to be reported. If the employer also needs assistance in calculating the membership data for reporting purposes refer to our Membership Calculation Service here.

